TOP STORY OF THE DAY, brought to you free by WICU: Comparing COVID-19 outbreak to that of Spanish Flu of early 1900s
Using data from the Centers for Disease Control and Prevention and the World Health Organization, the Brazil Times created the following comparison of the deadly Spanish Flu to the current COVID-19 pandemic.
SPANISH FLU OUTBREAK
During the officially estimated 820 days from 1918-1920, the Spanish Flu virus affected one-third of the world’s population (1.8 billion), with an estimated more than 500,000,000 infected (27.77%) and 50,000,000 deaths (2.777778% of the population) reported worldwide.
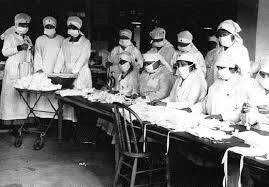
In America (103.2 million population), the virus, later identified as H1N1, is considered the most lethal in modern history, resulting in 650,000 deaths (.629845%). At the time, doctors didn’t know influenza viruses even existed. Medical technology, pharmacology, and diagnostic testing were limited or were not created. Penicillin was not invented until 1928, and there were no flu antiviral drugs available. Critical care measures, such as intensive care support and mechanical ventilation, also were not available in 1918.
Coordinated pandemic plans were non-existent in 1918; however, some communities implemented mitigation measures, such as wearing cloth face coverings, closing schools, banning public gatherings, and issuing isolation or quarantine orders.
The federal government took no centralized role in planning or initiating these interventions during the 1918 pandemic.
COVID-19 OUTBREAK
The current coronavirus pandemic - COVID-19 - originated in Wuhan, China, in December 2019. The first laboratory-confirmed case of COVID-19 was confirmed on January 20, 2020, in America, and reported to CDC two days later.
During the subsequent 346 days, current data available from the World Health Organization (data available on December 30, 2020) shows COVID-19 cases are increasing worldwide, infecting 83,264,353 (1.03556%) of the 7.8 billion people and 1,816,164 deaths reported (.229%).
In America, 19,432,125 COVID-19 cases (5.8707%) have been reported among the 331 million residents, with 337,419 deaths reported (.102%).
The available treatments, diagnostics, and technology for the current pandemic are more advanced than 100 years ago, including the availability of rapid testing, antiviral drugs, ventilators, and vaccines.
There are surveillance networks like the WHO and the CDC, which monitor seasonal flu viruses and the emergence of novel viruses while assisting countries worldwide.
The CDC issued general guidelines at the beginning of the pandemic in America to help slow the spread of the virus similar to those used during the Spanish Flu, including:
• Wear face coverings/masks
• Practice 6-foot social distancing
• Wash hands regularly with soap and water for 20 seconds, or use hand sanitizer with at least 60% alcohol for proper hygiene.
• Stay home in isolation if you are sick or are in close contact with someone who has COVID-19.
ANTI MASK DEBATE
A hundred years ago, the debate over masks began during the Spanish Flu pandemic, and it continues today.
When the Spanish Flu arrived in San Francisco in the fall of 1918, the city passed an ordinance requiring everyone to wear a mask while in public or a group of two or more people, except at mealtime. Failure of a person to wear a mask or not properly wearing one could lead to police warnings, charges of disturbing the peace, and subsequent violations of stricter fines or incarceration.
The first ordinance was annulled in November 1918, with a new one taking effect in January 1919. (This last ordinance was lifted February 1, 1919, on the Board of Health’s recommendation.)
The Anti-Mask League of San Francisco organized to protest the ordinance, although an estimated 80% of the residents initially complied.
The heated debate centered on objections the cloth masks were useless against the Flu, while others considered it an infringement of civil liberties. Making the issue even harder to understand, some health officers from other cities agreed that the masks were unnecessary.
A 1919 study muddied the water even more, stating that masks were not effective in the way expected. The conclusion cited the likely reason for the ineffectiveness: masks, made of inadequate materials, were only worn outdoors and not used inside in gatherings where conditions for transmission was higher.
In 2020, although medical historians have partly attributed the decline in deaths 100 years ago from the influenza pandemic in San Francisco to the mandatory mask-wearing policies, the COVID-19 mask guidelines have sparked another heated public debate.
Health officials are currently encouraging the public to wear cloth face coverings (preserving the more efficient N95 masks for frontline and healthcare workers). Masks are to be worn whenever they leave their homes to help mitigate coronavirus spread and practice 6-foot social distancing and maintain proper hygiene and handwashing.
APPLES TO ORANGES?
With 474 days to compare COVID-19 to the Spanish Flu outbreak, the data is expected to change significantly as health officials believe at least one more spike is on the horizon.
At the end of December 2020, Indiana State Department of Health’s data for Clay County continued to show a RED status with a high spread level.
Of the total population of 26,255 in Clay County during 2020, a little more than 17,000 people were tested, with 9,248 being tested once, and 1,907 confirmed to have COVID-19 since March. Most of the positive cases have or are currently in the recovery process. However, 31 deaths (the mot recent on Dec. 31 2020) have been confirmed related to COVID-19 complications.
